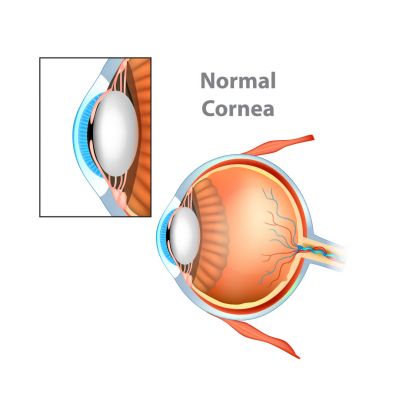
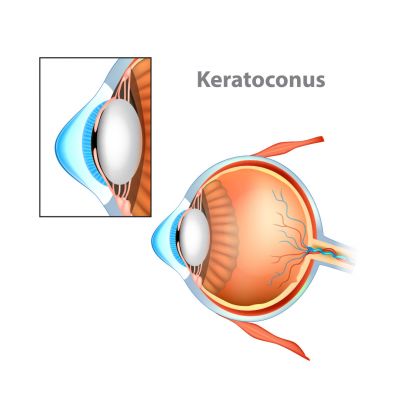
What is Keratoconus?
The fibres that make up the middle layer of the cornea (the transparent part of the eye) are weaker than normal, which causes the cornea to bulge and become distorted. Vision loses its sharp focus and reading and driving become difficult.
What causes Keratoconus?
There is no obvious single cause and it’s often associated with allergic conditions, such as eczema, asthma and hay fever. People with itchy eyes often rub them vigorously, and there is evidence that this rubbing can initiate or make keratoconus worse. It can be hereditary and is also more common in some ethnic groups.
How will it affect my vision?
Each person is different, but most find difficulty seeing small details. Some see distorted or multiple images, some are particularly sensitive to light, and vision is often difficult in the dark as lights can look like starbursts.
People with keratoconus will usually need glasses or contact lenses to correct their sight.
People with keratoconus will usually need glasses or contact lenses to correct their sight.
Progression
Keratoconus tends to start in the teens or twenties. It may stabilise after a short time or might continue for more than 20 years until finally stabilising. Progression is rare after the age of 35 years.
For some people it remains mild, but for others the progression advances to a stage where the cornea is very steeply curved and distorted. In about 2% of cases the back surface of the cornea splits, and the cornea becomes waterlogged and opaque. This is known as Hydrops – it can be painful but usually heals with time.
For some people it remains mild, but for others the progression advances to a stage where the cornea is very steeply curved and distorted. In about 2% of cases the back surface of the cornea splits, and the cornea becomes waterlogged and opaque. This is known as Hydrops – it can be painful but usually heals with time.
Treatment Options
Optical correction of vision
If the keratoconus affects one eye only, and the visual problems are slight, some patients may not want an optical correction. In the early stages, vision can be corrected with glasses and increases in distortion may require frequent change in glasses.
If the distortion is irregular, contact lenses are more successful, as they float on the surface of the cornea, replacing the distorted surface with a smooth surface which is able to focus the light accurately.
Rigid contact lenses are usually the first choice, as they give better visual results than soft lenses. However, other types of contact lenses, such as thick soft lenses (made especially for keratoconus), hybrid, “piggy back” or scleral lenses can also be used. The best type of lens can only be determined after an eye examination. Glasses and contact lenses do not slow down the rate of progression of the keratoconus, they just correct the vision.
If the distortion is irregular, contact lenses are more successful, as they float on the surface of the cornea, replacing the distorted surface with a smooth surface which is able to focus the light accurately.
Rigid contact lenses are usually the first choice, as they give better visual results than soft lenses. However, other types of contact lenses, such as thick soft lenses (made especially for keratoconus), hybrid, “piggy back” or scleral lenses can also be used. The best type of lens can only be determined after an eye examination. Glasses and contact lenses do not slow down the rate of progression of the keratoconus, they just correct the vision.
Medical / Surgical management
- Stabilising the progression: Corneal Collagen Cross Linking
If keratoconus shows progression, a surgical procedure known as corneal collagen cross linking may be used to slow or stop the condition getting worse by strengthening the cornea. This is not suitable for people whose Keratoconus has already stabilised. - Corneal ring segment inserts (Intacs or Kera rings)
Clear, thin ring inserts are slid between the layers of the cornea to alter the shape of the central cornea and make it less irregular. This requires adequate thickness and transparency of the cornea and may not be suitable for everyone. - Surgery to replace the cornea with donated corneal tissue: cornea transplant. This is only considered when contact lenses are no longer tolerable, or when the cornea has lost its transparency. The affected cornea is replaced by a clear one from a deceased person.
Copyright © 2019. Amit Patel